
ValueDX Approach
Discover AI-Powered Healthcare Agents — On Your Terms
Step into the ValueDX AI Experience Center and explore how intelligent automation is transforming denial prevention, denial tracking, and revenue recovery. Watch AI agents in action as they streamline workflows, eliminate manual tasks, and improve financial performance across your platform.
Key Capabilities
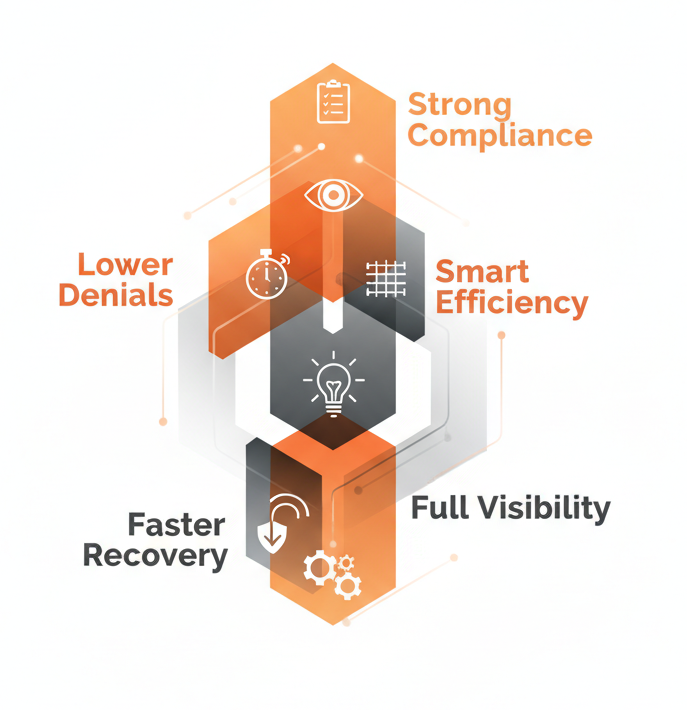
Business Value
Why choose valueDX
Experience the Power of Healthcare AI Agents Firsthand
Learn how ValueDX AI-powered agents can strengthen your denial management lifecycle, reduce administrative burden, and recover more revenue with less effort. Schedule a personalized demo designed for your RCM team’s unique challenges.
Fill out the form below and we’ll be in touch to schedule a convenient time.
Let’s explore how intelligent automation can transform your healthcare delivery.
FAQs
Before You Leave…
See how our Denial Management & Denial Tracking solutions can reduce write-offs, improve reimbursement, and enhance operational visibility.
Request a Free Consultation
