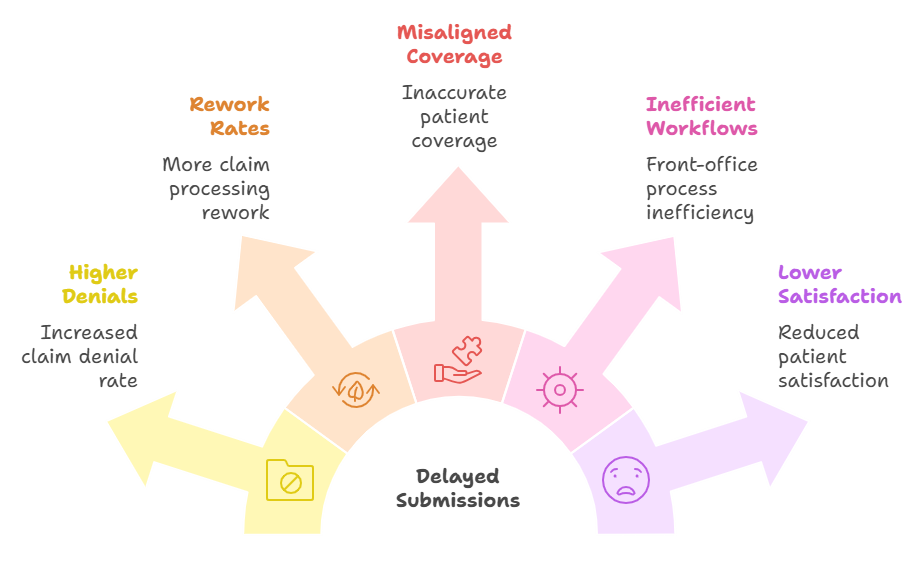
The Hidden Costs of Manual Eligibility Checks
Healthcare teams loose countless hours navigating payer websites, cross-checking data and updating records manually.
Discover AI-Powered Healthcare Agents — On Your Terms
Step into the ValueDX AI Experience Center and witness our intelligent automation solutions in action.
Experience how AI-powered eligibility and revenue agents eliminate manual data entry, improve payer accuracy, and accelerate claim approvals — all in real time.
The Foundation of Clean Claims Starts Here

Eligibility and benefits verification are the first and most critical steps of revenue cycle success. Manual checks across payer portals often lead to outdated data, missed coverage, and claim rejections. With ValueDX Eligibility AI, verification becomes instant, accurate and automated across all major payers.
Digital Specialist for Eligibility Verification
The ValueDX AI Eligibility Agent automates the entire verification workflow — retrieving, validating and updating insurance data in real time. It continuously learns payer behavior, detects invalid policies and ensures that billing begins with clean, verified data.
End-to-End Eligibility Automation in Action
ValueDX automation engine securely connects to payers and clearinghouses to perform high-speed, high-accuracy verification.
Real-Time Accuracy. Measurable ROI.

HIPAA-Compliant and Audit-Ready
ValueDX ensures all eligibility workflows adhere to HIPAA, SOC 2 and ISO 27001 standards. All patient and payer data is encrypted, logged and auditable — meeting the highest standards for healthcare data security.

Purpose-Built for Healthcare Workflows
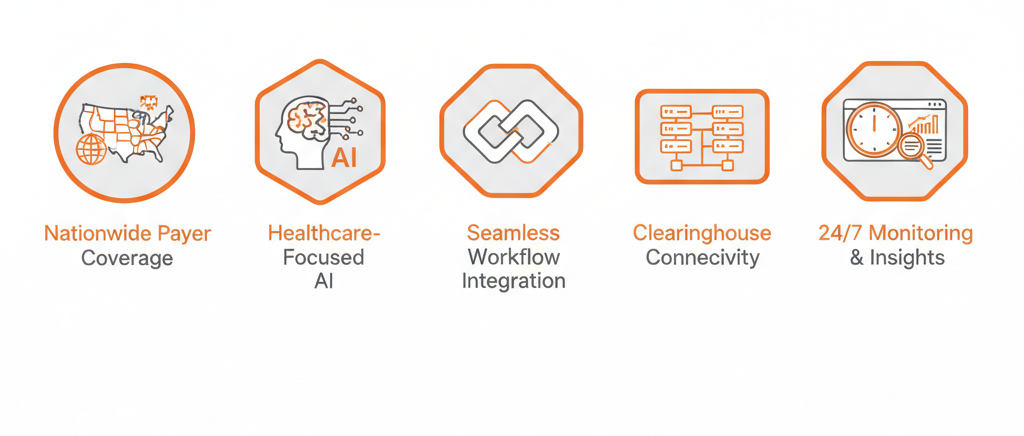
Seamless Integration with Your Systems
ValueDX connects effortlessly with your EHR, practice management and billing platforms for automatic verification updates
Experience the Power of Healthcare AI Agents Firsthand
See how ValueDX AI-powered agents can transform your healthcare platform—reducing administrative burdens, elevating patient experience, and accelerating cash flow.
With deep integrations across EHRs, payers, and clearinghouses, our AI agents empower data-driven decisions and proactive revenue intelligence for sustainable growth.
Fill out the form below and we’ll be in touch to schedule a convenient time.
Let’s explore how intelligent automation can transform your healthcare delivery.
FAQs
Before You Leave…
Discover how AI-powered eligibility verification can reduce claim denials, accelerate approvals, and improve revenue cycle performance.
Request a Free Consultation
